Taking the ‘ouch’ out – effect of buffering commercial xylocaine on infiltration and procedure pain – a prospective, randomised, double-blind, controlled trial
Younis I, Bhutiani RP
Supported by Decades of Clinical Research
Studies consistently show that pH-balanced local anesthetics provide improved comfort and much faster onset of anesthesia

A large body of research shows that removing the acid from local anesthetics produces faster onset, less injection pain, and increased reliability1.
An April 2023 study2 published in the British Journal of Oral and Maxillofacial Surgery showed consistent results, and is especially notable because of the large number (n=108) of patients and statistical power of the results.
Numerous studies, published in peer-reviewed journals, have concluded that pH-balanced (also referred to as “buffered” and “alkalinized”) results in a significant improvement in injection comfort, speed of onset, and reliability of anesthesia vs. un-buffered anesthetic.

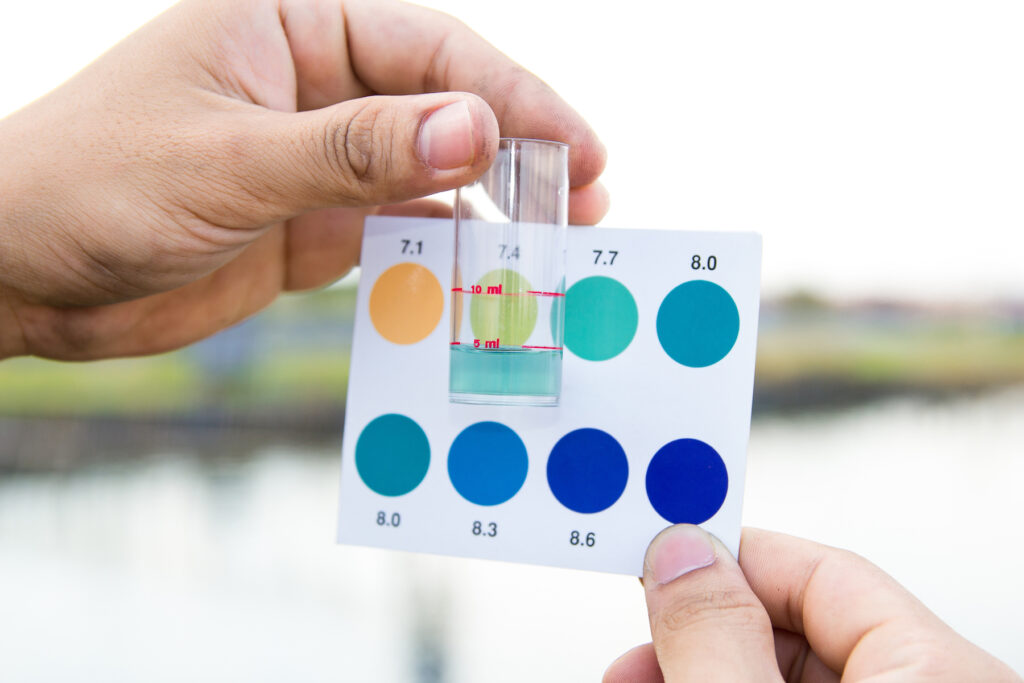
The anesthetic in dental cartridges has an acidic pH of about 3.9, compared with tissue pH of 7.4. Normally, after injection, the body buffers the local anesthetic toward physiologic pH, which eventually increases the availability of the active form of the anesthetic. This ultimately leads to nerve blockade (“numbness”).
It has also been demonstrated that balancing the pH significantly reduces the painful burning sensation. There are two possible mechanisms by which increasing the pH of an anesthetic could decrease the pain associated with its injection.
Increasing the pH increases the amount of anesthetic in uncharged form, which could either be less irritating to the tissues than the charged form or, alternatively, be capable of entering the nerve sheath much more rapidly than the charged form, thereby blocking pain transmission almost instantaneously.


Burns and colleagues3 attributed the improvement in injection comfort through balancing the pH to both:
They concluded the following:
In addition, at a lower pH, less of the anesthetic is in its active, freely diffusible form, leading to a prolonged time until onset of anesthesia. In a more neutral, buffered solution, the area is anesthetized more quickly and further infiltration is less painful3.
When sodium bicarbonate solution is mixed with a local anesthetic, the reaction will, among other things, create water (H2O) and carbon dioxide (CO2).
Condouris and Shakalis showed that this CO2 possesses an independent anesthetic effect. Catchlove concluded that the independent anesthetic effect of CO2 may provide the most immediate form of analgesia4.
Given that Burns, Richtsmeier, and Talu attribute reduced injection pain to the rapidity with which pain signals are blocked when using buffered anesthetic, Catchlove’s finding may also point to a mechanism by which buffering with sodium bicarbonate reduces injection pain.

Published Research
Studies on the science of pH balancing or buffering
Want a Better Dental Anesthetic?
Join the growing list of clinicians who want this new technology available as soon as possible.
* Products are currently in development, and are not approved by FDA for sale or distribution. Please stay tuned for updates.
THIS WEBSITE MAY CONTAIN FORWARD-LOOKING STATEMENTS AND INFORMATION RELATING TO, AMONG OTHER THINGS, THE COMPANY, ITS BUSINESS PLAN AND STRATEGY, AND ITS INDUSTRY. THESE FORWARD-LOOKING STATEMENTS ARE BASED ON THE BELIEFS OF, ASSUMPTIONS MADE BY, AND INFORMATION CURRENTLY AVAILABLE TO THE COMPANY’S MANAGEMENT. WHEN USED IN THE OFFERING MATERIALS, THE WORDS “ESTIMATE,” “PROJECT,” “BELIEVE,” “ANTICIPATE,” “INTEND,” “EXPECT” AND SIMILAR EXPRESSIONS ARE INTENDED TO IDENTIFY FORWARD-LOOKING STATEMENTS, WHICH CONSTITUTE FORWARD LOOKING STATEMENTS. THESE STATEMENTS REFLECT MANAGEMENT’S CURRENT VIEWS WITH RESPECT TO FUTURE EVENTS AND ARE SUBJECT TO RISKS AND UNCERTAINTIES THAT COULD CAUSE THE COMPANY’S ACTUAL RESULTS TO DIFFER MATERIALLY FROM THOSE CONTAINED IN THE FORWARD-LOOKING STATEMENTS. INVESTORS ARE CAUTIONED NOT TO PLACE UNDUE RELIANCE ON THESE FORWARD-LOOKING STATEMENTS, WHICH SPEAK ONLY AS OF THE DATE ON WHICH THEY ARE MADE. THE COMPANY DOES NOT UNDERTAKE ANY OBLIGATION TO REVISE OR UPDATE THESE FORWARD-LOOKING STATEMENTS TO REFLECT EVENTS OR CIRCUMSTANCES AFTER SUCH DATE OR TO REFLECT THE OCCURRENCE OF UNANTICIPATED EVENTS.
(1) “Over 90% Of Dentists Report A Desire For Current Anesthetics To Be More Reliable, Less Painful, Or Faster Acting,” Olson Research Group, “Dentist Quantitative Report, Conducted For Balanced Pharma, August 13, 2021,” Fielding: June 18–July 19, 2021, Total Sample Size: N=181
(2) “Effectiveness of Buffered and Non-Buffered Local Anesthetic in Inferior Alveolar Nerve Block: A Randomised Study”, M Bala, A.O. Taiwo, A.A. Ibikunle, H.O. Olasoji, A.O. Sulaiman, B.C. Chukwuma, R.O. Braimah, B.O. Ileogedengbe, Published in the British Journal of Oral and Maxillofacial Surgery, April 21, 2023; https://www.bjoms.com/article/
(3) Burns CA, Ferris G, Feng C, Cooper JZ, Brown MD, “Decreasing the pain of local anesthesia: a prospective, double-blind comparison of buffered, premixed 1% lidocaine with epinephrine versus 1% lidocaine freshly mixed with epinephrine”, J Am Acad Dermatol. 2006 Jan;54(1):128-31
(4) Richard F. H. Catchlove, “The Influence of CO2 and pH on Local Anesthetic Action“, Journal of Pharmacology and Experimental Therapeutics May 1972, 181 (2) 298-309
(5) “58% Of Patients Believe The Injection Is The Worst Part Of The Dental Experience,” Olson Research Group, “Patient Dental Care Study Quantitative Report, Conducted For Balanced Pharma, May 7, 2021,” Fielding: March 30–April 23, 2021, Total Sample Size: N=140 (Includes 40 Parents/Caregivers)
(6) 2018 Meta-Analysis: Significantly Decreased Onset Time And Injection Pain; Guo Et Al From University Of Southern California School Of Dentistry Concluded: “Buffered Lidocaine Significantly Decreased Onset Time And Injection Pain (Vas) Compared With Non-Buffered Lidocaine In Inferior Alveolar Nerve Block.”; 2017 Clinical Study: Reduces The Pain On Injection; Phero Et Al From University Of North Carolina School Of Dentistry Concluded: “Buffered Lidocaine Reduces The Pain On Injection With A Maxillary Field Block And Results In Similar Lengths Of Pulpal Anesthesia As Non-Buffered 2% Lidocaine.” 2017 Clinical Study: Lower Pain On Injections. Warren Et Al From University Of North Carolina School Of Dentistry Concluded: “After Mandibular Nerve Block, Buffered 1% Lidocaine Can Produce Similar Duration Of Pulpal Anesthesia As Non-Buffered 2% Lidocaine And Lower Pain On Injections.”; 2019 Meta-Analysis: 2.29 Times More Reliable In Inflamed Teeth; Kattan Et Al From University Of Pennsylvania School Of Dentistry Concluded: “Buffered Local Anesthetics Have 2.29 Times Greater Likelihood Of Achieving Successful Anesthesia [In Pulpally Involved Teeth].”
(7) BPI Owns The Following Granted Patents And Pending Patent Applications: U.S. Patent No. 11,305,064 (Issued April 19th, 2022); U.S. Application No. 17/722,016; International Pct Application No. Pct/Ib2018/052598; Canadian Application No. 3,111,347 (Canadian National Phase Of Pct/Ib2018/052598); European Application No. 18897951.2 (European Regional Phase Of Pct/Ib2018/052598); Japanese Application No. 2020-556351 (Japanese National Phase Of Pct/Ib2018/052598); Korean Application No. 10-2020-7021685 (Republic Of Korea National Phase Of Pct/Ib2018/052598); U.S. Application No. 16/655,362; U.S. Application No. 63/233,879; Bpi Also Owns One Trademark Application, U.S. Application No. 88/198,808, Pending For The Libracaine Mark.